Georgia: a primary health care case study in the context of the COVID-19 pandemic
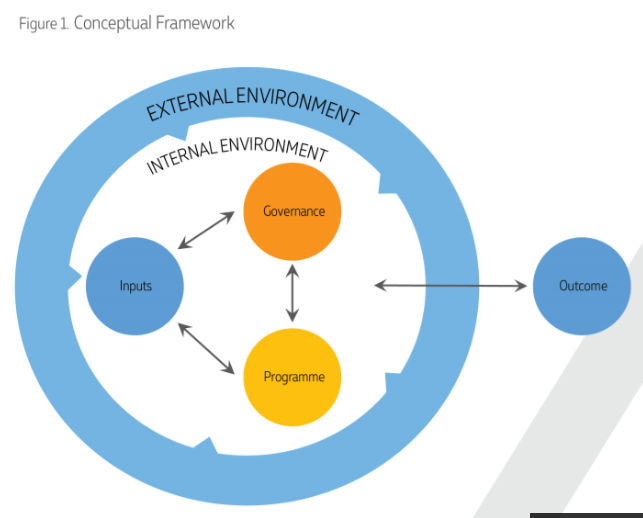
 The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
The Government of Georgia reacted to COVID-19 with timely and coordinated response activities that delayed the arrival of the first COVID-19 case in the country and slowed spread of the infection during the first wave of the epidemic. The government’s multisectoral actions were coordinated by the Interagency Coordination Committee (ICC) under the Prime Minister’s leadership, with the ICC serving as the main decision-making platform. An effective public health response was guided by the Ministry of Health and the National Center for Disease Control and Public Health (NCDC), and was implemented through coordinated efforts that spanned different sectors.
At the time of the country’s first confirmed case of COVID-19, the primary care system was not yet ready to serve as a first contact level for patients with suspected infection. To avoid an influx of patients at primary care facilities and mitigate the risks of infection, people were asked to use the ambulance service or self-refer to designated hospitals that had greater capacities for infection prevention and control.
Meanwhile, drawing on Georgia’s experience during the 2018–2019 flu epidemic, an online consultation service was established, based in 25 PHC facilities. Their primary tasks were patient triage, remote home-based management and follow- up. This service was gradually expanded to 60 PHC facilities, and was supported with trainings and methodological guidance, different reimbursement schemes and quality monitoring mechanisms.
The establishment of the patient pathways, with clear roles for the emergency hotline (112), online clinics, ambulance service and referral points was critical to ensure safe access to the services that were needed. During the second wave of the epidemic, the operation of online clinics under central online clinic supervision ensured the management of most COVID-19 cases and prevented the collapse of the system.
Georgia’s routine primary care services did not stop during the COVID-19 pandemic. All essential preventive and curative services were retained, although physical visits were replaced in many cases by online consultations – a pattern that was more common in urban than in rural areas. However, mobility restrictions and fears of contracting COVID-19 had a negative impact on the use of services such as immunization, cancer screening and tuberculosis diagnostics. In addition, community engagement in the COVID-19 response was weak, as it lacked the active involvement of community groups in discussions and in two-way dialogue with the government.
The pandemic also revealed long-standing structural problems with primary care such as the fragmentation of care, shortages of human resources, weak capacities in infection prevention and control, and an underdeveloped health management information system (HMIS). The pandemic revealed that strong PHC plays an essential role in mitigating risks and reducing pressures on the entire health system. By exposing the weakness the system, the pandemic has catalysed major changes for its future improvement.
Assessment of PHC in the country is essential to draw lessons and to inform the design of multisectoral preparedness plan for future public heath emergencies. Moreover, the COVID-19 response learnings can be considered in the design of the planned primary care reform.
Latest News
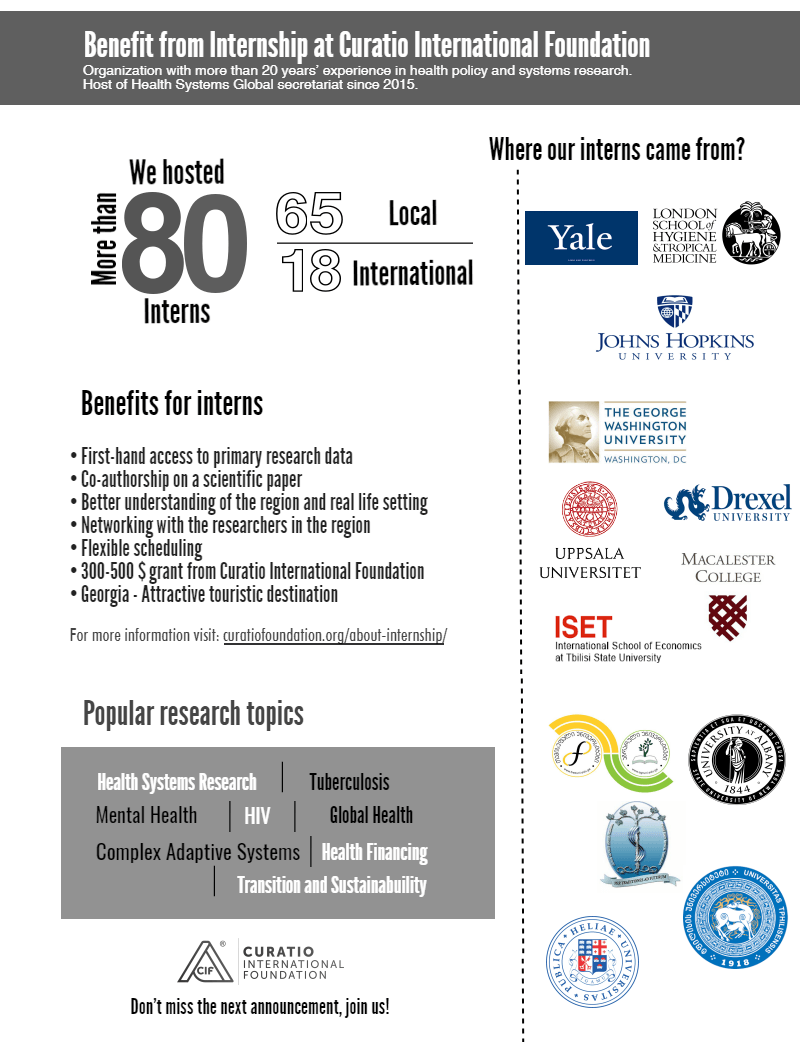
2025-2026 Winter Internship Program
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
New Paper: Breaking Barriers to Universal Health Coverage: Insights from Georgia’s Chronic Disease Medicine Program
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
New Paper: From fragmented to functional: Improving rehabilitation data in Georgia’s health information systems for better decision-making
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
New Paper: Counting the savings: impact of Georgia’s drug policy interventions on households
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
New Paper: Financial protection and universal health coverage in Georgia: an analysis of impoverishing healthcare costs using household income and expenditure surveys
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Countries Unite in Manila to Strengthen Advocacy for New Vaccine Introduction through Collaborative Learning
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Integrated Bio-behavioral surveillance and population size estimation survey among Female Sex Workers in Tbilisi and Batumi, Georgia, in 2024
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Curatio International Foundation at Eighth Global Symposium on Health Systems Research (HSR2024)
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
“The Informatics and Data Science for Public Health: Sustainment Plan for Skilled Labor Force Development”
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Janina Stauke from the London School of Hygiene and Tropical Medicine shares her internship experience
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Jolly Mae Catalan fromUniversité Libre de Bruxelles shares her internship experience
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Georgia’s Journey to Integrating Rehabilitation Services into the Health System: Insights and Lessons
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Report on Rehabilitation Data Flow in Georgia’s Health Information System
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Adult vaccination in Asia and the Pacific
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Assessment of the Quality of Maternal and Neonatal Services in Montenegro
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Barometer Study: Pharmaceutical Sector in Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Call for Internship 2024
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Georgian state rehabilitation program: implementation research study report
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
NEW Barometer, study focusing on the pharmaceutical sector
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Strengthening Health Systems for Accessible Rehabilitation Services in Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Linked’s workshop on HPV vaccine introduction and scale up, held on July 11-12th, 2023
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Training program focusing on interdisciplinary evaluation of rehabilitation interventions and patient outcomes
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Unlocking Success Through Learning: Workshop on Strengthening HR Capacity and Performance Management in Immunization
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Promote evidence-based policies in the pharmaceutical sector by generating evidence and fostering civic engagement
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
CIF and the Results for Development / Accelerator combined their expertise to co-author an insightful blog, shedding light on Georgia’s commendable efforts to overcome limited data challenges and develop evidence-based policies for financing rehabilitation services
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Culminating event – Building Institutional Capacity for Health Policy and Systems Research and Delivery science (BIRD) in six WHO Regions
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Report on Phased (Stepwise) Plan for the Capability Development of the Priority Rehabilitation Services
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Report on prioritization of rehabilitation services in Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Report on Rehabilitation Service Costing and Budgeting
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Mental health of young people during the COVID-19 pandemic
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Promote evidence-based policies in the pharmaceutical sector by generating evidence
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Mandatory Vaccination and Green Passes – Review of International Experience
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Sustaining Public Health Gains after Donor Transition: What can we learn about Georgia?
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Curatio International Foundation at Seventh Global Symposium on Health Systems Research (HSR2022)
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Curatio International Foundation at Global Symposium on Health Systems Research
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
EECA HIV Sustainability Summit 2022 in Tbilisi
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Study report: Adaptations made in TB response during Covid-19 pandemic in Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
New review of our recent study on Immunization in Kazakhstan
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
New case study: Sustaining effective coverage with Opioid Substitution Therapy (OST) in Georgia in the context of transition from external assistance
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
New case study: National Immunisation Program Transition from external assistance
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
“Strengthening Health Systems for Accessible Rehabilitation Services in Georgia” – Workshop
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Strengthening the Delivery of Immunisation Services Through PHC Platforms-Workshop
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Call for internship 2022
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
New Article published in the journal Frontiers in Public Health
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
New Paper: A transdiagnostic psychosocial prevention-intervention service for young people in the Republic of Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Vaccine Procurement and Supply for the Expanded Program of Immunization in Kazakhstan
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Prevention of Addiction and Mental Health in Adolescents in Georgia (PAMAd) – Workshop
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Workshop to discuss the risk assessment of future TB migrants
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Webinar : Matters of Scale and Integration in Digital Health Ecosystems
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Immunisation Action Network
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Data Analysis and Synthesis Workshop – analyzing the implications of the structure of Georgia’s private healthcare market for quality and accessibility
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
External Reference Pricing Policy: A Possible Pharmaceutical Price Regulation Policy in Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Rapid reviews of health policy and systems evidence
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Paper: Soviet legacy is still pervasive in health policy and systems research in the post-Soviet states
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Strategic Fellowship – series of training courses for students
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
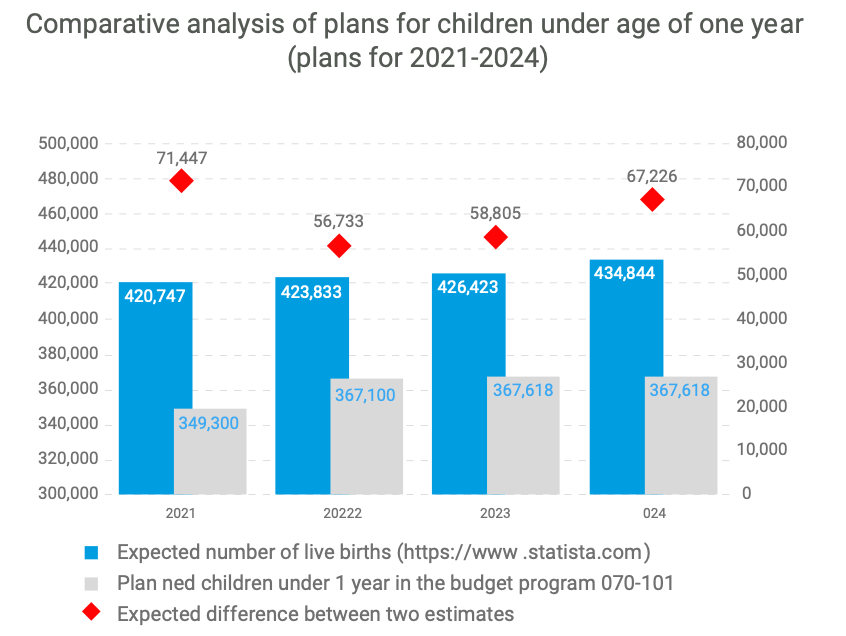
Georgian NIP faces challenges in sustaining the outcomes achieved
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
CIF Internship Program 2021
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Enroll to the CIF’s Strategic Fellowship Programme
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Article: How do participatory methods shape policy? Applying a realist approach to the formulation of a new tuberculosis policy in Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Bundled Payment Methods: An Alternative Payment Method to Contain Healthcare Costs in Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
HOW TO MAINTAIN ROUTINE IMMUNIZATION DURING COVID-19? EXPERIENCES FROM ARMENIA, GEORGIA, AND UZBEKISTAN
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
DRUG CHECKING: An Essential Response to Emerging Harm Reduction Needs
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
GEORGIA COVID-19 VACCINE COMMUNICATIONS CAMPAIGN TO ADDRESS HESITANCY ISSUES
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Supporting Evidence-Informed Policy making and Action in Six WHO Regions
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Georgian Healthcare Barometer XIV Wave The analysis of financial stability and risks in healthcare
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Call for educational Strategic Policy Fellowship Program
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
We are pleased to announce that The Sixth Global Symposium on Health Systems Research (HSR2020) has opened
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Discussing interim results of research project: Prevention of Addiction and Mental Health in Adolescents in Georgia (PAMAd)
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Effects of Pay for Performance on utilization and quality of care among Primary Health Care providers in Middle and High-Income countries
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Does pay for performance work to improve immunization coverage?
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
CAN SOCIAL MEDIA MONITORING LEAD TO IMPROVED PERCEPTIONS ABOUT IMMUNIZATION?
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
The first phase of the joint fellowship program of the Curatio International Foundation and the Knowledge to Policy Center (K2P) at the American University of Beirut has been successfully implemented
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
LNCT WEBINAR: Incremental Costs of Routine Immunization, Campaigns, and Outreach Services During COVID-19
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
LNCT Webinar: Assessing Bottlenecks to Adequate and Predictable Vaccine Financing
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
LNCT WEBINAR: Designing Behavioural Strategies for Immunization in a Covid-19 Context
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Concentration and fragmentation: analyzing the implications of the structure of Georgia’s private healthcare market for quality and accessibility (ConFrag)
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
LNCT Discussion Group: COVID-19 Impact on Immunization Programs
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
#COVID19 – Evidence and Policymaking: Personal Reflections from an LMIC Setting
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
The COVID-19 epidemic in Georgia Projections and Policy Options
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Modeling of Four Possible Scenarios of COVID-19 epidemics in Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Application for Summer Internship program is closed
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
LNCT Webinar: Key Considerations for Integrating Immunization with Other Primary Health Care Services
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Georgia Sharing knowledge to Armenia to strengthen immunization legislation
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Call for Interns as researchers is now open
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Improving access to pharmaceuticals in Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
LNCT Webinar: Addressing Vaccine Hesitancy Challenges
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
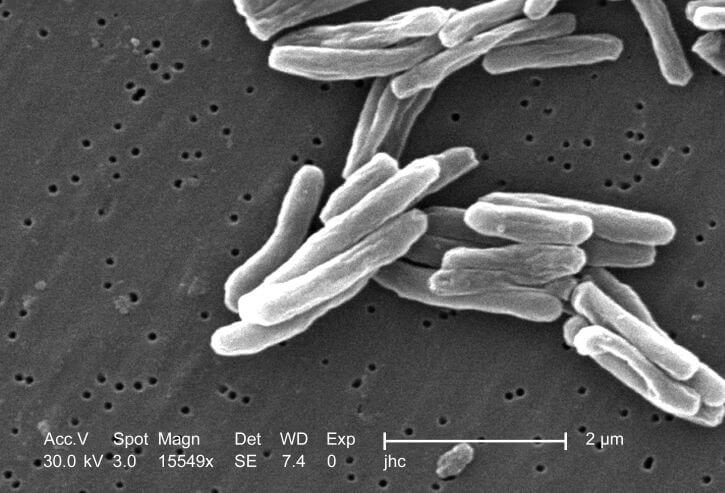
Project on “Technical Assistance Using Modern Technology for TB Prevention, Diagnosis, and Increased Quality Treatment” was closed
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Dialogue on Pharmaceutical pricing policies to improve the population’s access to pharmaceuticals in Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
LNCT Webinar: Implementing a High Performing Immunization Program within the Context of National Health Insurance: What can we Learn from Thailand?
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
LNCT Webinar: Strengthening Public-Private Engagement for Immunization Delivery
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Implementing new research: Prevention of Addiction and Mental Health in Adolescents in Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Georgia’s introduction of the Hexavalent vaccine: Lessons on successful procurement and advocacy
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Georgia Primary Health Care Profile: 6 Year after UHC program introduction
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
National consultations to propose a new model of TB funding
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
HSR2020: RE-IMAGINING HEALTH SYSTEMS FOR BETTER HEALTH AND SOCIAL JUSTICE
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
CALL FOR MENTEES: PUBLICATION MENTORSHIP FOR FIRST-TIME WOMEN AUTHORS IN THE FIELD OF HPSR
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
A pilot of a new intervention launched to Improve adherence to TB treatment and its outcomes in Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Training for epidemiologists and health workers on TB contact tracing new guideline
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Workshop on using modern technology for TB prevention, diagnosis and increased quality treatment
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
K2P Mentorship Program on Building Institutional Capacity on Evidence Informed Policy Making
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Training on using Research Evidence for Policy Making
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Doing embedded development and research – reflections on the start of the Results4TB programme
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Healthcare Advocacy Coalition (HAC) for Human Oriented Healthcare
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Introductory Meeting on the project ‘Embedding Rapid Reviews in Health Policy-Making’
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Taavy Miller from University of North Carolina shares her internship experience
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Building Institutional Capacity for HPSR and Delivery Science- CIF is Europe region HUB
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Inter-regional workshop in preparation for transitioning towards domestic financing in TB, HIV and Malaria programmes
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Memorandum of Cooperation between the Health and Social Issues Committee of the Parliament of Georgia and Curatio International Foundation
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Embedding Rapid Reviews in Health Systems Decision-Making (ERA)
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Curatio International Foundation at the Global Symposium on Health Systems Research
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
The civil society gathered for the fourth time to discuss healthcare system challenges in Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Project: HIV risk behavior among Men who have Sex with Men – Bio-Behavioral Surveillance Survey and Population Size Estimation
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Curatio International Foundation at AIDS2018
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Big Pharma Greed and Artificial Prices – Knocking on Door to Limit Access to HIV Medicines in Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Civil society is gathering for the third time to hold a discussion about the healthcare
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Webinar: Gavi Vaccine Prices Post-Transition
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Webinar: Mapping and consensus of global competencies set for the field of HPSR: A progress update and HSG round table discussion
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Health Systems Global Publishes Annual Report 2017
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Webinar: Vaccine Forecasting and Budgeting Tools and Best Practices
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Technical Assistance for evaluation of transition readiness and preparation of Transition and Sustainability Plan for Global Fund-supported programs in Tajikistan
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Technical Assistance for the preparation of Transition and Sustainability Plan for HIV program in Philippines
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Discussing the accessibility of medicines in Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Webinar: Integrating gender into health system strengthening in conflict and crisis-affected settings; what’s in our toolkit?
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Article: Barriers to mental health care utilization among internally displaced persons in the republic of Georgia: a rapid appraisal study
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Why Georgians second-guess their doctors – Deregulation has left Georgian medical care something many Georgians would rather avoid
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Ara Srinagesh from New York University Shares her Internship Experience
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Webinar on The peer review process – what happens when you send your manuscript to a journal
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Webinar on Improving Quality of Care during Childbirth: Learnings and Next Steps from the BetterBirth Trial
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Civil Society is Being United to Discuss Healthcare System Issues
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Curatio International Foundation for a TB-Free World
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Summer Internship Program is now open
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Closing Project: Tuberculosis Community Systems Strengthening in Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Primary Health Care Systems: Georgia case study
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
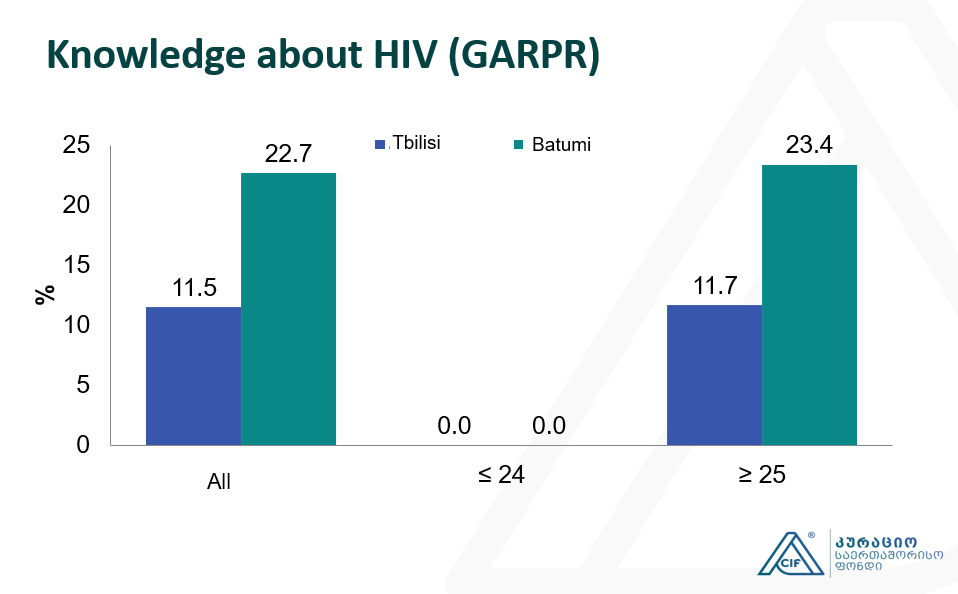
Integrated Bio-behavioral surveillance and population size estimation survey among Female Sex Workers in Tbilisi and Batumi, Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Applying a Health Policy and Systems Research lens to Human Resources for Health: Capacity building, leadership and politics
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
CIF hosts Aradhana Srinagesh throughout the winter internship program
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
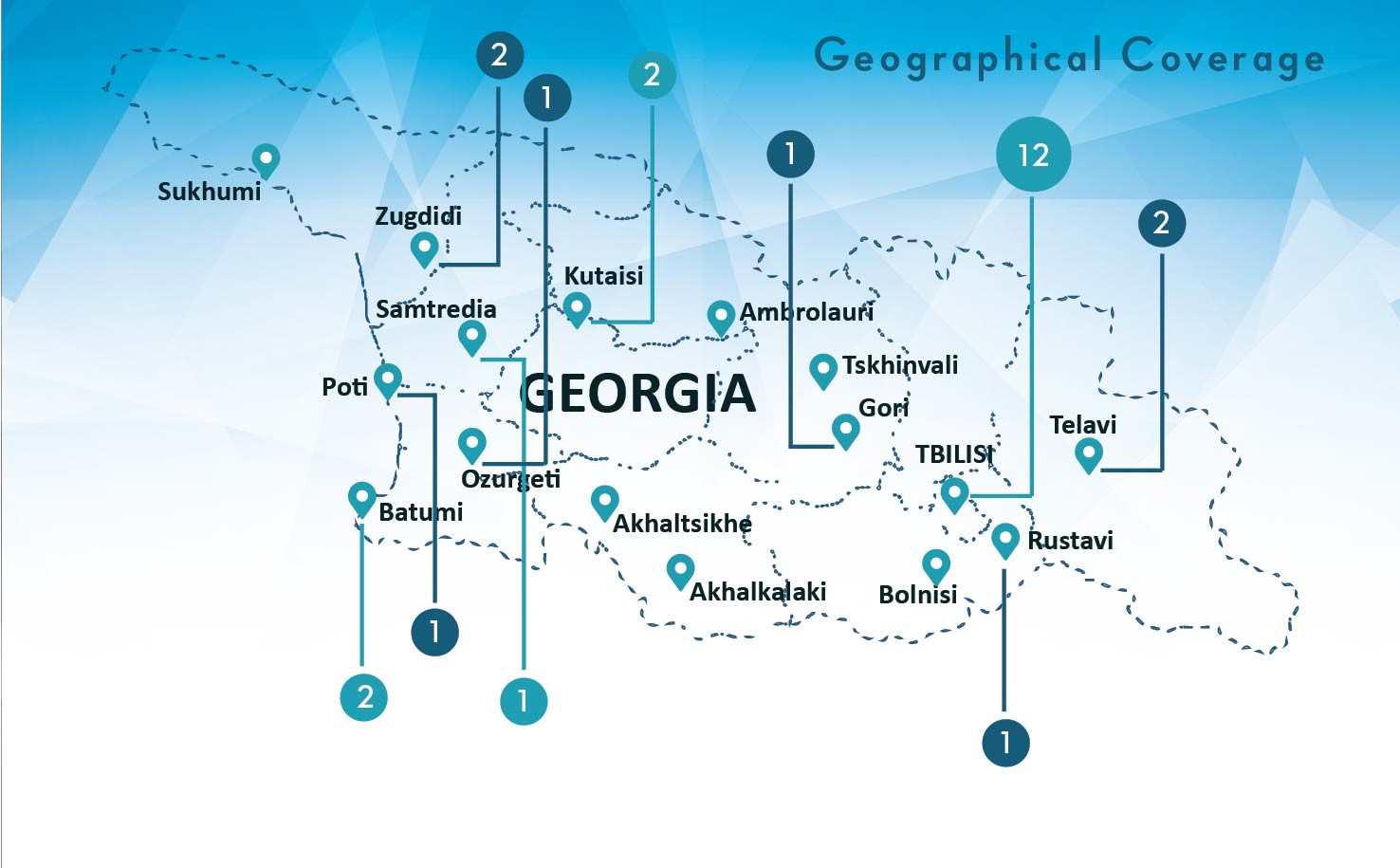
Empowering civil society for engagement in and monitoring the decision making in health sector in Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Curatio International Foundation presented BBS and PSE study findings at the Civil Society Forum
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
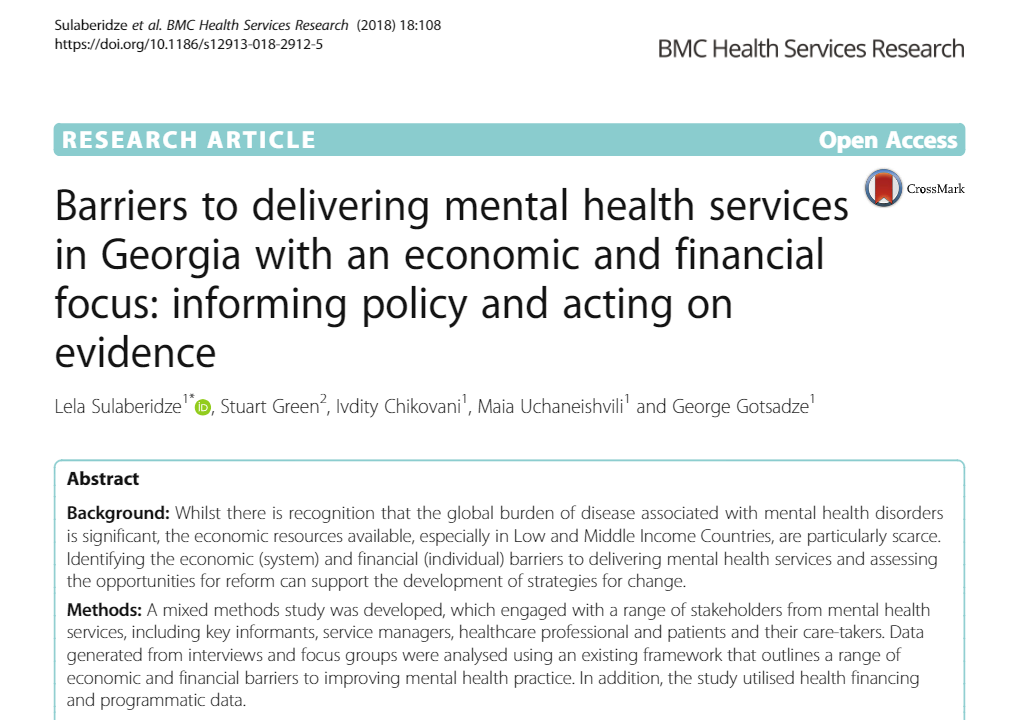
Article: Barriers to delivering mental health services in Georgia with an economic and financial focus: informing policy and acting on evidence
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
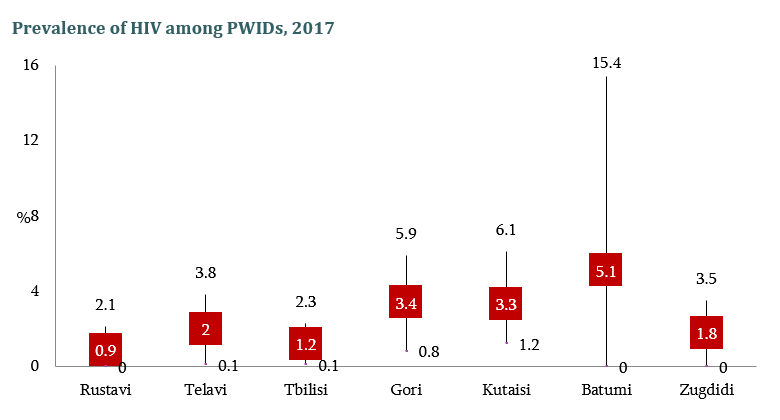
The Interview on population size and Human Immunodeficiency Virus risk behaviors of People who Inject Drugs in Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Population Size Estimation of People who Inject Drugs in Georgia 2016-2017
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
HIV risk and prevention behaviors among People Who Inject Drugs in seven cities of Georgia, 2017
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
#WorldAIDSDay2017
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Conference paper: The Study of Barriers and Facilitators to Adherence to Treatment among Drug Resistant Tuberculosis Patients in Georgia to Inform Policy Decision
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Article: Human immunodeficiency virus prevalence and risk determinants among people who inject drugs in the Republic of Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Conference paper about realist evaluation: Informing policy, assessing its effects and understanding how it works for improved Tuberculosis management in Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Georgian Healthcare and its Challenges: Healthcare Expert George Gotsadze will host the lecture
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
17 years in Curatio International Foundation: President Ketevan Chkhatarashvili to Leave Organization
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Be ready for the Best Internship Experience
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Apply for Our Winter Internship Program
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Georgian Solution for a Post-Soviet TB Program: Can Integration into Primary Health Care Improve TB Care?
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Moving Forward: Second PT workshop with TB stakeholders in Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Article: Determinants analysis of outpatient service utilization in Georgia: can the approach help inform benefit package design?
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Designing and evaluating provider results-based financing for tuberculosis care in Georgia (RBF4TB)
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Forbes Georgia: The Importance of Evidence in Decision Making
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Barriers and Facilitators to Adherence to Treatment Among Drug Resistant TB Patients in Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Summer internship program 2017 is open now!
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Transition Preparedness Assessment
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
New Study Findings About Tuberculosis
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Meet CIF in Vancouver at HSR2016
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Curatio International Foundation: Transition and Sustainability Portfolio
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Article: Privilege and inclusivity in shaping Global Health agendas
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Eastern Europe and Central Asia Regional Sustainability and Transition Coordination Summit 20-21 October, 2016 Vilnius, Lithuania
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Internship Announcement, Winter 2016-17
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Evaluation of UNICEF’s Contribution in Central and Eastern European Five Countries
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
CIF researchers represented on Global Conference AIDS2016
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
UHC 2030: Building an Alliance to Strengthen Health Systems
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
CIF Pharmaceutical Price and Availability Study (Fifth Wave Results)
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Assessment of GAVI Alliance HSS support to Tajikistan
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Final Evaluation of Gavi’s Support to Albania
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Infographic: HIV/AIDS in Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
HIV risk and prevention behaviours among Prison Inmates in Georgia, 2015
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Washington DC hosts workshop Immunization Costing: what have we learned, can we do better?
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Bio-Behavioral Surveillance Survey among Men who have Sex with Men in two major cities of Georgia, 2015
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
EPIC Studies – Governments Finance, On Average, More Than 50 Percent Of Immunization Expenses, 2010–11
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Bio-Behavioral Surveillance Survey among People Who Inject Drugs in 7 cities of Georgia, 2015
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
TB Community Systems Strengthening in Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
What can be done to improve treatment adherence among tuberculosis patients in Georgia: Looking through health systems lens
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Summer Internship Program 2016
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
BioBehavior Surveillance Survey results were represented to the members of Parliament of Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Announcing Winter Internship Program 2016
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Regional High Level Dialogue ‘Road to Success’, Tbilisi, Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
CIF study results on 8th IAS Conference on HIV Pathogenesis, Treatment and Prevention
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Response to the “Final evaluation of GAVI support to Bosnia and Herzegovina”
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
The drivers of facility-based immunization performance and costs. An application to Moldova
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Awaiting the results of Prisoners’ Behavior Surveillance Survey (BSS)
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Costs of routine immunization services in Moldova: Findings of a facility-based costing study
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Analyses of Costs and Financing of the Routine Immunization Program and New Vaccine Introduction in the Republic of Moldova
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Health Service Utilization for Mental, Behavioural and Emotional Problems among Conflict-Affected Population in Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Healthcare Utilization and Expenditures for Chronic and Acute Conditions in Georgia: Does benefit package design matter?
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Curatio International Foundation Hosts Health Systems Global Secretariat in Tbilisi, Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
An Impact Evaluation of Medical Insurance for Poor in Georgia: Preliminary Results and Policy Implications
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Policy Information Platform (PIP) Expert Consultation Meeting
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Civil Society Forum organized by Country Coordination Mechanism
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Drexel University on CIF Internship Program
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
CIF Publishes the Short Movie on 20 Years of Healthcare, 2014
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
CIF Publishes Anniversary Publication ’20 Years of Health Care, 2014
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
CIF Celebrated the 20th Anniversary
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Georgian Healthcare System Barometer: Experts’ Evaluations of Changes Taking Place in the Healthcare
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
BlogTalkRadio to Host CIF President
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Winner of CIF Students Fellowship Program for 2013-2014
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Mental Health Among IDPs in Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
The Forbes and Skoll World Forum to discuss HIV/AIDS Epidemic with Director of CIF
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
CIF Participation in the Private Sector in Health Symposium 2013
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Article on Springer-Determinants of Risky Sexual Behavior Among Injecting Drug Users in Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Tobacco Use and Nicotine Dependence among Conflict-Affected Men in the Republic of Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
HIV prevalence and risk behaviors among key populations- Study Findings Published
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Think Tanks Signed an Ethical and Quality Standards Document
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Hosting interns from international universities
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Hosting interns from international universities
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
CIF’s contribution to Investing in Global Health and Development
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
CIF Fellow Awards Event
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Assessing the Health Insurance for the Poor in Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Curatio International Foundation Among Grant Management Solutions Awarded Partners
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Fourth Wave Results of Pharmaceutical Study Published
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
CIF Calls for participation in internship program for 2012-2013
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Curatio International Foundation revealed the winner of its annual scholarship program
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Impact of global HIV/AIDS initiatives on health systems in Ukraine, Kyrgyzstan and Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Submission of Applications for CIF Scholarship for Master Program Students near to deadline
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Health care in Georgia is currently available for very rich and very poor
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Presentation of the findings of Assessment of Complex Non-Communicable Condition in Low Income Countries
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Poster Presentation at Copenhagen 2012 Conference on HIV
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Contributing to publishing the paper: Circus monkeys or change agents? Civil society advocacy for HIV/AIDS in adverse policy environments
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
National Center for Biotechnology Information published CIF’s scientific paper on Unsafe injection and sexual risk behavior among injecting drug users in Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Findings of the pharmaceutical market study in 2009-2011 years
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Main findings of Catastrophic Health Expenditure Analysis in Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Contribution to the development of National Health Care Strategy 2011-2015
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Catastrophic Health Expenditure Analysis in Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
New web guide for using qualitative approaches to health systems research
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
CIF Study Published in BMC Magazine, The Role of Supportive Supervision on Immunization Program Outcome- a randomized filed trial from Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
CIF Calls for participation in internship program for 2011-2012
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Releasing results of Bio-behavioral surveillance survey among men having sex with men
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Winner of the Fellowship Program 2011 Revealed
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Prices, Availability and Affordability of Medicines in Georgia-the New Study Report Endorsed
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Customer Satisfaction Research Report on Corporate Health Insurance Released
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Statement for the Media-The Study on Injected Drug Users Completed
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
National and subnational HIV/AIDS coordination: are global health initiatives closing the gap between intent and practice?
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Assessment of HIV/AIDS Surveillance System Pilot is Already Available
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Findings of Behavior Surveillance Surveys (BSS) Endorsed
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Internship at Curatio International Foundation is challenging for John Hopkins University Students
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
The Art of Crafting Policy Briefs
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Representatives of CIF Visit 2010 Global Health Information Forum
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Training in Evidence Search-Acquisition
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Marking 15th Anniversary
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Hosting Club Discussion on Mental Health Policy
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Put Final Touches on the Training in Policy and Political Cycle
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
A New Paradigm for Regulating Georgian Pharmaceutical Market
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
CIF will Launch Fellowship for the Best Student of Healthcare/Public Health Management Faculty
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
CoReform Project and the Ministry of Health Mark the Completion of the First Stage of Trainings on ICPC2 Application
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Georgia HIS Strategic Plan posted on Health Metrics Network website
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
First Stage of Training Course on Evidence Informed Policy Formulation Crowned
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Findings of Behavior Surveillance Surveys (BSS) to be Endorsed Soon
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
The Study on System-wide Effects of the Global Fund on Georgia’s Health Care Systems posted on GHIN website
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Behavior Surveillance Survey among CSWs Covers Batumi and Tbilisi
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Sentinel Surveillance Method to Provide Reliable HIV/AIDS Statistical Data
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Curatio International Foundation Contributes to Global HIV/AIDS Initiatives
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Mr. George Gotsadze approved as a Permanent Member of the Global Fund TRP
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
The research article on Household Catastrophic Health Expenditure-evidence from Georgia and its policy implications published in BMC Health Services Research
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
CIF Hosts workshop on Classifications for Hospital and Laboratory intervention
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
National Conference in the framework of the Global Fund funded project
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
CIF conducted a workshop to discuss HIV/AIDS Surveillance System Assessment results
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
CIF conducted a workshop in the framework of the project funded by the Global Fund
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
The Global Fund Contracted Curatio International Foundation for Consulting Services
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
CIF and MoLHSA conduct a workshop on Integrated Model and Strategic Plan for the Health Information system development in Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Regional Workshop on Rotavirus and Diarrheal Disease
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
National Avian Influenza Surveillance Guidelines
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Dr. George Gotsadze – CIF director and PATH board member presented “Hope for health in a weakened nation”
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Natia Rukhadze – CIF Researcher at the Global HIV/AIDS Initiatives Network (GHIN) international workshop in Dublin, Ireland
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
George Gotsadze – CIF director at fifth Global NHA symposium in Lund, Sweden
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Yale University Announced Selection of Leading Georgian Public Health Expert, Ketevan Chkhatarashvili, as a 2007 Yale World Fellow Yale University announced the selection of the leading Georgian health policy advisor, Ketevan Chkhatarashvili, the preside
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Introductory Workshop on National Health Accounts in Azerbaijan
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Armenia Visit Report
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Protocol of the Policy Club on the Public Health Organizational Development
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Ukraine Mission Report
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Health Research for a Responsive Healthcare System in Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Development of Hospital Master Plan for Georgia, 1998-1999
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Hospital Financing in Georgia: Problems & Solutions, 1998-1999
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Healthcare Reform in Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.
Final Report on Family Planning and Reproductive Health Assessment in Georgia
The case study examines primary health care (PHC) in the context of the COVID-19 pandemic in Georgia between January 2020 and July 2021. The Astana PHC components are used to consider integrated integrated primary care and essential public health functions, and essential public health functions, community engagement and multisectoral collaboration. A desk-based review was conducted, supplemented by a trend analysis of secondary data.